Diabetes means constantly monitoring your food intake and blood sugar levels and managing the relentless highs and lows. Even when you’re doing everything right, something can still feel off. Persistent stomach issues, mood swings that disrupt your day, and overwhelming exhaustion that goes beyond the typical diabetes battle might be familiar experiences to you.
The truth is that diabetes affects your gut, which plays a significant role in your overall well-being. It can disrupt the communication between your stomach and brain, impacting your mood, energy levels, and long-term health.
The Gut-Brain Axis
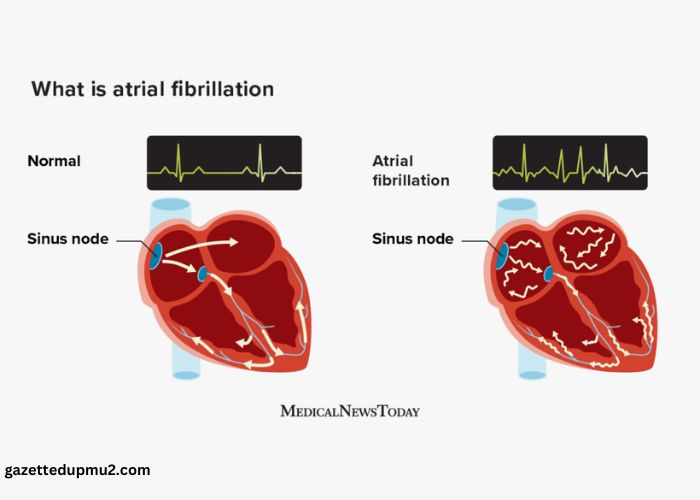
Your gut plays a far more complex role than simple food digestion. It houses a vast network of bacteria, nerves, and signaling chemicals. This system, known as the gut-brain axis, maintains constant two-way communication with your brain, influencing your mood, stress responses, and overall well-being.
Messages travel along the gut-brain axis in several ways. Gut bacteria produce neurotransmitters, primarily GABA, NE, DA, 5-HT, and histamine, that directly communicate with the brain. The vagus nerve, a significant information pathway, also connects the gut and brain.
Inflammation triggered by gut imbalances can negatively impact brain function. Studies suggest that an imbalance in gut bacteria may contribute to anxiety, depression, cognitive decline, sensitivity to pain, and other mood disorders.
Disruptions in the gut-brain axis can create a vicious cycle for individuals with diabetes. Gut imbalances and mood disturbances can make blood sugar control more challenging, exacerbating inflammation and perpetuating the problem.
Understanding this connection highlights the potential benefits of gut-focused interventions for improving physical and mental health in diabetes.
How Diabetes Harms the Gut and Your Well-Being
A healthy gut requires diverse bacteria, but diabetes can disrupt this balance. This leads to the overgrowth of harmful microbes, which compromises digestion, weakens the immune system, and triggers inflammation that makes blood sugar control even harder.
This inflammation damages the gut lining (making it “leaky”) and harms the brain, leading to worsened mood and reduced mental clarity. Additionally, high blood sugar can damage nerves over time, including those that control stomach function. This condition, called gastroparesis, prevents the stomach from emptying properly, causing bloating, nausea, vomiting, and constant fullness.
Gastroparesis makes blood sugar control unpredictable because food absorption becomes erratic. Gut bacteria changes contribute to cravings and energy crashes and increase long-term health risks. Additionally, since the gut influences mood, feeling physically unwell takes a significant mental toll.
While essential for managing diabetes, some medications can trigger or worsen gut problems. Research from the University of British Columbia indicates that GLP-1 agonist medications like Ozempic increase the risk of conditions such as gastroparesis, pancreatitis, and bowel obstruction.
Researchers found that people taking GLP-1 medications have a 9.09 times higher risk of pancreatitis, a 4.22 times higher risk of bowel obstruction, and a 3.67 times higher risk of gastroparesis. Although these events are rare, the widespread use of these drugs means thousands of people could be affected.
For example, many people using Ozempic to treat diabetes experience persistent gastrointestinal problems like stomach paralysis, vomiting, and gallbladder issues. Unaware of these potential side effects, some individuals have filed an Ozempic lawsuit against the manufacturer, Novo Nordisk. These lawsuits allege that the company failed to warn about the risks associated with the drug adequately.
If you’re experiencing severe gut problems after taking Ozempic, you may be eligible to take legal action. As per TruLaw, U.S. District Judge Gene E. K. Pratter in Philadelphia oversees the consolidation of these cases. As of February 2024, 55 lawsuits have been consolidated, and the litigation is in its preliminary stages.
The Impact on Mood, Stress, and More
When you have diabetes, feeling down goes beyond occasional bad days. Studies show that around 39.5% of diabetic patients experience depressive symptoms compared to 12.4% of non-diabetics, and 36.2% of diabetic patients suffer from anxiety compared to 14.4% of non-diabetics. This isn’t just temporary sadness; it can impact relationships, energy levels, and the ability to manage the demands of diabetes itself.
The stress of the gut-brain connection triggers a cascade of physical changes in your body. This worsens blood sugar control, which then adds to your stress levels. Meanwhile, gut problems caused by diabetes become a constant source of anxiety and discomfort, fueling an endless loop.
Research suggests a growing link between diabetes and an increased risk of cognitive decline later in life, including conditions like dementia and Alzheimer’s disease. This decline can be slow and progressive, affecting people of all ages, though it’s more common in older individuals.
An unhealthy gut sends distress signals to the brain, contributing to feelings of unease, irritability, and difficulty focusing. When you add this to the burden of diabetes management, it’s easy to see why mental health might take a backseat. However, addressing gut health alongside standard diabetes care can be key to improving your mood.
Protecting Your Gut, Protecting Your Mind
Improving your gut won’t cure diabetes, but it can make a big difference in how you feel physically and mentally. Focus on whole, unprocessed foods and plenty of fiber to nourish healthy gut bacteria. Your doctor or a dietician can offer specific advice tailored to your diabetes needs.
Stress directly affects digestion and your microbiome. That’s why mind-body practices like meditation, yoga, or even short breathing breaks can offer significant benefits.
Openly discuss any gut issues with your doctor, especially if they started after medication changes. There may be ways to adjust your treatment plan for better blood sugar control and improved gut comfort.
FAQs
How Do I Know if My Gut Is Unhealthy?
If you experience frequent digestive problems like gas, bloating, constipation, or diarrhea could signify an unhealthy gut. Additionally, unexplained weight changes, fatigue, skin issues, and mood swings can be linked to an imbalanced gut microbiome.
What Part of the Brain Is Responsible for Gut Feeling?
A single brain area doesn’t control gut feelings. Instead, they result from a complex interaction between several regions. Primarily, the anterior insula (aINS) and the orbitofrontal cortex (OFC) play vital roles. They process information from the gut and emotional and cognitive signals, ultimately shaping that intuitive “gut feeling” sensation.
What Are the Symptoms of Gut Brain Dysfunction?
Symptoms of gut-brain dysfunction can vary, but the most common include abdominal pain, bloating, constipation, diarrhea, indigestion, and feelings of food getting stuck in the throat.
How Can I Improve My Gut-Brain Axis?
To bolster your gut-brain axis, prioritize a fiber-rich diet (fruits, vegetables, whole grains), include fermented foods (yogurt, kimchi), consider probiotics, and manage stress levels. Exercise and adequate sleep are also beneficial for fostering a healthy gut microbiome, promoting positive communication between your gut and brain.
Wrapping up, living with diabetes, and feeling overwhelmed by how it affects both your body and mind is a lot to handle. But small steps toward better gut health can make a real difference in your well-being.